Article

Asthma can make everyday activities — like running, playing, or even laughing a little too hard — a challenge for some children (1). Traditional asthma treatment has long focused on medication, but there’s another piece of the puzzle that’s often overlooked: pulmonary rehabilitation (PR).
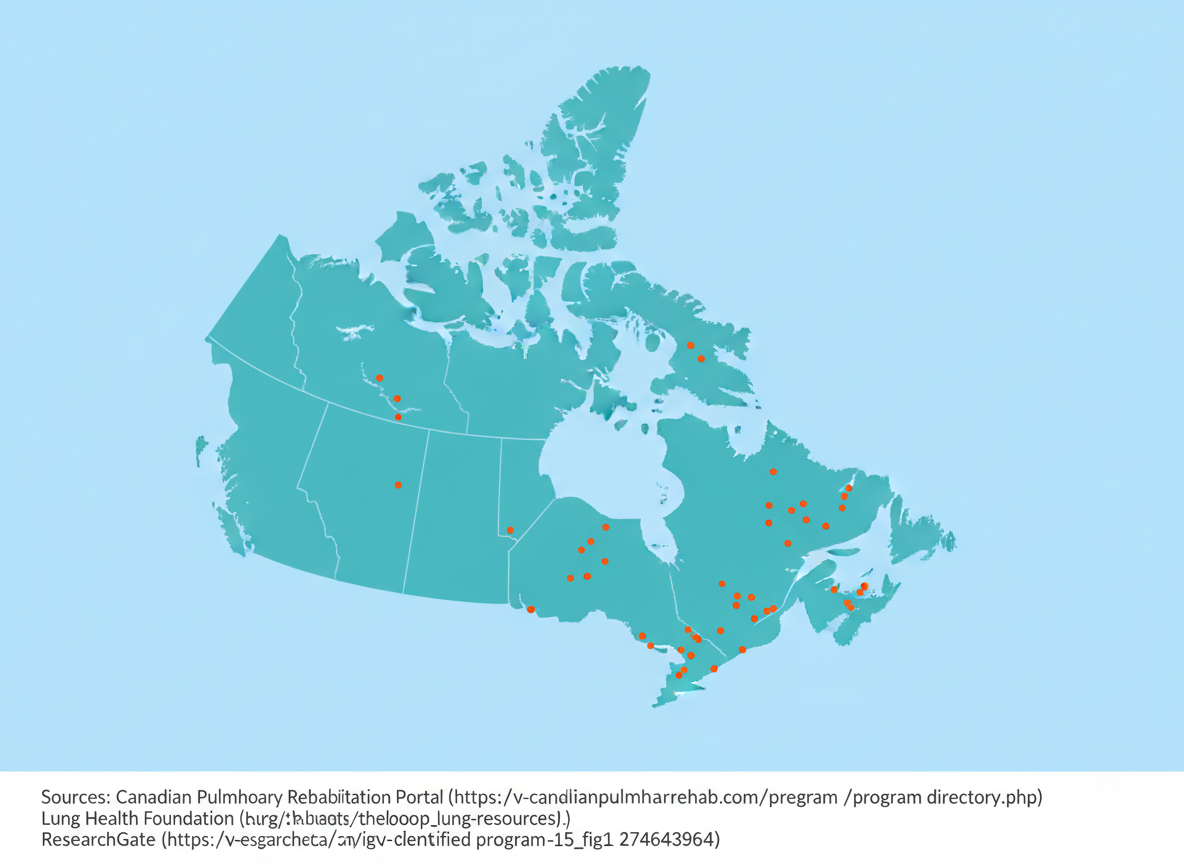
Despite being the most common chronic respiratory disease in children around the world, pulmonary rehabilitation (PR) has not been well explored as a pediatric treatment tool for asthma (2, 3). Most PR programs have been focused on adults with chronic obstructive respiratory disorder (COPD), but there has recently been more research looking into the benefits of PR in children.
Let’s take a look into what it is, how it works, and how it can help your child breathe easier!
What Is Pulmonary Rehabilitation?
Pulmonary rehabilitation is a multidisciplinary program that combines:
- Exercise training
- Education
- Breathing techniques and breath training
- Lifestyle and behavioural change
Together, these components help people with chronic respiratory conditions improve their health, manage symptoms, and enhance overall quality of life (4–6).
PR programs are specially designed to promote changes that are supportive of long-term respiratory health (2).
How Pulmonary Rehabilitation Helps Children With Asthma
Although PR is more established in adult care, pediatric research is beginning to reveal several promising benefits.
Studies have shown that pulmonary rehabilitation and exercise training can lead to improvements in lung function, inspiratory muscle strength, asthma control, and quality of life for children and caregivers alike (1, 2, 7, 8). Some studies have reported that PR can also improve exercise performance although this result is still up for debate (1, 2, 8).
Where Does the Research Stand?
Overall, the evidence shows that pulmonary rehabilitation is a promising and viable option for improving quality of life and lung function in children with asthma (3, 6).
Not all studies show improvements across every measure (1, 2, 8). For example, one study found benefits in inspiratory muscle strength, asthma control, and quality of life, but not in spirometry or exercise capacity (2). PR may need to be tailored specifically for pediatric patients, and more research is needed to determine best practices for children of different ages, asthma severities, and fitness levels.
Despite these gaps, PR remains a valuable tool that could complement traditional asthma treatments.
The Bottom Line
Pulmonary rehabilitation is emerging as a powerful ally in pediatric asthma care. While medication remains essential, PR can support children by improving their lung function and quality of life, boosting confidence during physical activity, and enhancing daily quality of life.
As research grows, parents and clinicians alike may begin to see PR as a core part of asthma management — not just for adults, but for children too.
- Abdelbasset WK, Alsubaie SF, Tantawy SA, Abo Elyazed TI, Kamel DM. Evaluating pulmonary function, aerobic capacity, and pediatric quality of life following a 10-week aerobic exercise training in school-aged asthmatics: a randomized controlled trial. Patient Prefer Adherence 12: 1015–1023, 2018. doi: 10.2147/PPA.S159622.
- Yang S, Zhang Z, Liu Y, Liu E, Luo Z. The Effects of Combined Respiratory Muscle and Exercise Training in Children with Bronchial Asthma: A Randomised Controlled Study. J Asthma Allergy 16: 293–303, 2023. doi: 10.2147/JAA.S398108.
- Ma Q, Lu M, Yang Q, Gong F, Zhou L, Xu D. Effects of aerobic exercise-based pulmonary rehabilitation on quality of life in pediatric asthma: A systematic review and meta-analysis. Heart & Lung: The Journal of Acute and Critical Care 69: 11–30, 2025. doi: 10.1016/j.hrtlng.2024.09.005.
- Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, Hill K, Holland AE, Lareau SC, Man WD-C, Pitta F, Sewell L, Raskin J, Bourbeau J, Crouch R, Franssen FME, Casaburi R, Vercoulen JH, Vogiatzis I, Gosselink R, Clini EM, Effing TW, Maltais F, van der Palen J, Troosters T, Janssen DJA, Collins E, Garcia-Aymerich J, Brooks D, Fahy BF, Puhan MA, Hoogendoorn M, Garrod R, Schols AMWJ, Carlin B, Benzo R, Meek P, Morgan M, Rutten-van Mölken MPMH, Ries AL, Make B, Goldstein RS, Dowson CA, Brozek JL, Donner CF, Wouters EFM. An Official American Thoracic Society/European Respiratory Society Statement: Key Concepts and Advances in Pulmonary Rehabilitation. Am J Respir Crit Care Med 188: e13–e64, 2013. doi: 10.1164/rccm.201309-1634ST.
- Rochester CL, Alison JA, Carlin B, Jenkins AR, Cox NS, Bauldoff G, Bhatt SP, Bourbeau J, Burtin C, Camp PG, Cascino TM, Dorney Koppel GA, Garvey C, Goldstein R, Harris D, Houchen-Wolloff L, Limberg T, Lindenauer PK, Moy ML, Ryerson CJ, Singh SJ, Steiner M, Tappan RS, Yohannes AM, Holland AE. Pulmonary Rehabilitation for Adults with Chronic Respiratory Disease: An Official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med 208: e7–e26, 2023. doi: 10.1164/rccm.202306-1066ST.
- Wu P, Hu Y, Yan X. Progress in Research into the Effectiveness of Pulmonary Rehabilitation in Children with Asthma - A Narrative Review. J Asthma Allergy 17: 743–750, 2024. doi: 10.2147/JAA.S475367.
- Kirkby S, Rossetti A, Hayes D, Allen E, Sheikh S, Kopp B, Patel A. Benefits of pulmonary rehabilitation in pediatric asthma. Pediatric Pulmonology 53: 1014–1017, 2018. doi: 10.1002/ppul.24041.
- Bingöl Karakoç G, Yilmaz M, Sur S, Ufuk Altintas D, Sarpel T, Güneter Kendirli S. The effects of daily pulmonary rehabilitation program at home on childhood asthma. Allergol Immunopathol (Madr) 28: 12–14, 2000.
Related articles







Stay Informed
Receive the latest News and Blogs from Lung Games International
Receive biweekly updates from Lung Games International and stay informed about upcoming events.
Neem contact met ons op
Thank you for your message. We will respond as soon as possible.









