Info for Clinicians
The Need
- Asthma is the most common chronic condition in children, affecting 10 – 20% of children in Canada
- Canadian data show preschool children with asthma comprise over between 20% to 50% of ED consultations in this age group. 10% result in admissions and 1/25,000 will die
- Gap in early and accurate diagnosis as children < 6 years old often cannot perform conventional spirometry. Community clinicians often rely on symptoms, clinical history, and bronchodilator challenge, resulting in over and under estimation of control and severity
- With extensive coaching and gamified support in Pulmonary Function Labs, only 54% of preschool children can do spirometry. In addition, only 54% of individuals over 7 years of age received a pulmonary function test between 1 – 2.5 year from the initial incident to confirm diagnosis, and only 4.5% with asthma had received a PFT to monitor progress


Teaches Spirometry through Interactive Gaming – Sparky™ is an innovative game designed for preschoolers, leveraging human factor engineering. Using a portable spirometer as a game controller, it teaches children the breathing maneuvers required for spirometry through fun, interactive gaming. Target metrics are based on American Thoracic Society guidelines and the Global Lung Index neutral equations.
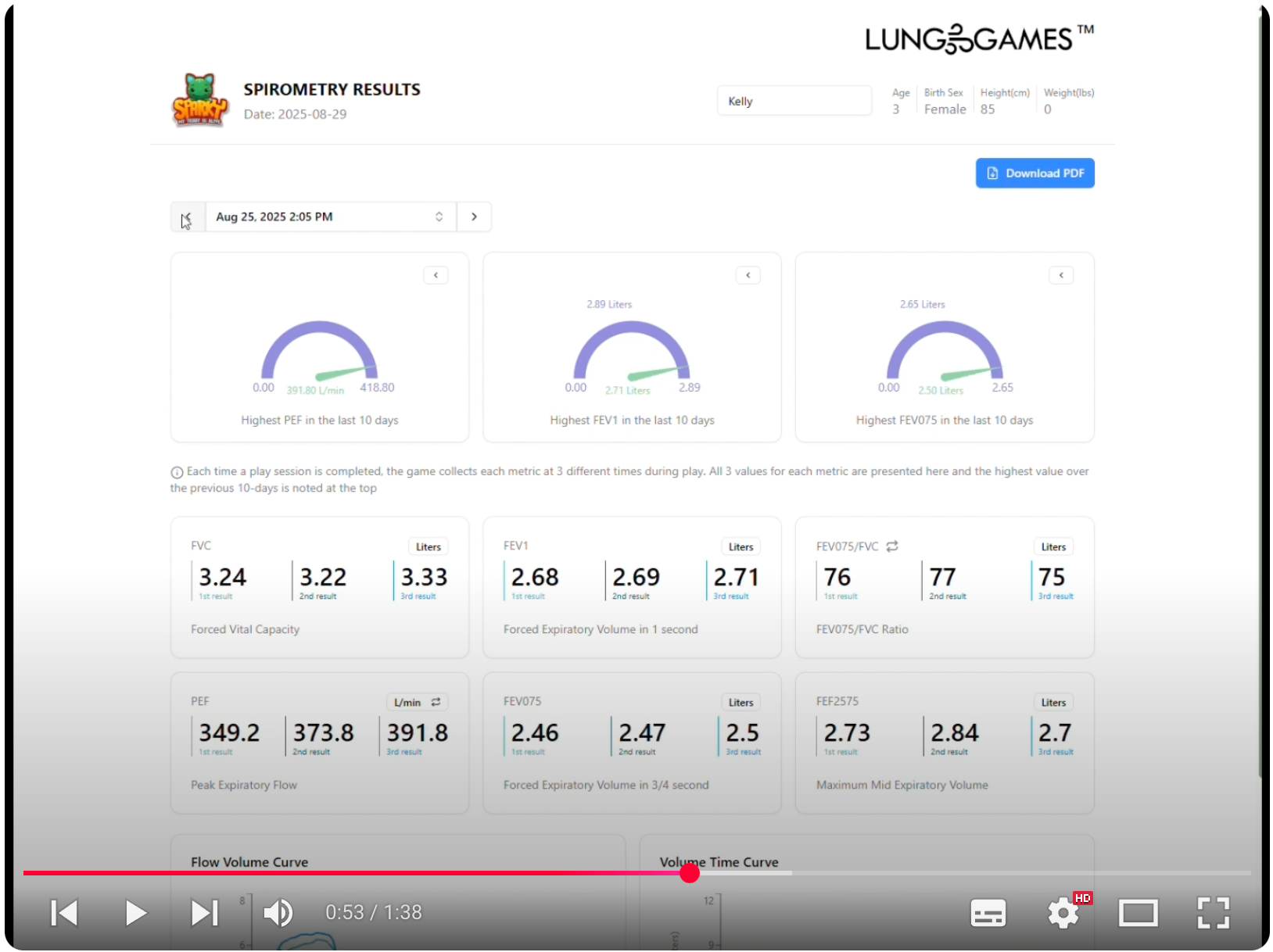
Remote monitoring and Objective, longitudinal Lung Function Data – Sparky™ tracks the key metrics for children (PEF, FEV1, FEV0.75, FVC, FEF2575, and ratios) with every game session, providing real-time data to support early diagnosis and monitoring. Parents and Clinicians can monitor remotely, or parents can print and provide progress reports.
Support the Asthma Action Plan and Increase Access to Care with Remote Monitoring
- With objective data, Clinicians can bridge the gap and rely on more than symptoms and clinical history to support care. Some Asthma Action Plans include PEF monitoring and now it’s possible, whether they live in the city or in rural and remote areas. Early intervention means potentially reducing ED and hospital admissions.
References:
- Canadian Paediatric Society – Managing an Acute Asthma Exacerbation in Children
- Health Quality Ontario – Case for Improvement (Slide deck - Evidence Document)
- Gaffin – Clinically useful spirometry in preschool-aged children: evaluation of the 2007 ATS Guidelines
- Asthma Canada – 2024 Annual Report
- Yang – Misdiagnosis of asthma in schoolchildren
- Kanj – Application of Global Lung Function Initiative Global Spirometry Reference Equations across a Large, Multicenter Pulmonary Function Lab Population
- Davis – Real-World feasibility of short-term, unsupervised home spirometry in CF
- Sarikloglou – Prediction of Asthma Exacerbations in Children
- Institute for Clinical Evaluative Sciences – Only a third of children with asthma treated in an Ontario ED seek recommended follow-up care
- Government of Canada – Asthma in Canada
- To – Did emergency department visits in infants and young children increase in the last decade? An Ontario. Canada study
- AAFA Asthma Facts and Figures
- Rochester – Insufficient Patient Access to Pulmonary Rehabilitation: A multifaceted problem







